Warning: This article contains discussion of suicide which some readers may find distressing.
A 21-year-old man diagnosed with a condition so painful it’s nicknamed the ‘suicide disease’ has opened up on what it’s like to live with it.
When Charlie Moore landed a place on a video editing apprenticeship scheme with MTV at the age of 18, he dropped out of college and relocated to London in order begin the course.
However his world would come crashing down during his second year of the course when he began to experience muscle spasms and tension in his right side, which then turned into ‘muscle-ripping’ pain along his right side.

21-year-old Charlie Moore had been looking forward to a career in video editing and filmmaking when he developed the debilitating condition (SWNS)
The pain would become so unbearable that Charlie was forced to drop out of his apprenticeship and move back in with his parents in Frome, Somerset – with doctors struggling to diagnose his condition over the following four years.
The confusion would last until just weeks go, when Charlie finally received a diagnosis for complex regional pain syndrome (CRPS) back in October.
What is complex regional pain syndrome (CRPS)?
According to the NHS, CRPS is a condition in which a person suffers from severe and debilitating pain.
Typically triggered by an injury, CRPS is often confined to one specific limb – however, it can spread to other parts of the body. Symptoms include muscle spasms, difficulty sleeping, intense pain and swelling in the affected area.
Charlie said: “I mainly get it in my right arm, right hand, it spreads all the way up into my shoulders, neck muscles and my head.
“All the muscles pull on each other when they go into spasm.”

The condition forced him to drop out of his apprenticeship and move back in with his parents (SWNS)
The condition’s other name is referring to some with the condition having suicidal thoughts as a result of the immense pain, the NHS says.
There is currently no cure for CRPS, however, doctors can help patients manage the pain through a variety of treatments.
For Charlie, his treatment will include starting a course of nerve blocks – which involves injecting medicine into the nerves to block pain signal – and physiotherapy.
Some people may show signs of improvement after a couple of years, but sometimes this is not always the case.
For Charlie, he would spend the years leading up to his diagnosis visiting A&E 10 times ‘begging’ for support from medical staff as he struggled with the excruciating pain.
Revealing the extreme measures the pain drove him to, he said: “I thought the pain would go away – but it became so extreme, I ended up attempting suicide.”

Following his diagnosis, the 21-year-old is now hoping the rebuild his life (SWNS)
“It just kept getting worse – I ended up having to drop out of my apprenticeship,” he continued. “I had to move back in with my family.”
Following his diagnosis, Charlie is now living with his parents and receiving £115-a-month Universal Credit and he is raising money to pay for his treatment and live independently via GoFundMe.
“I’m now in a position where I need to be getting back on track with my career,” he added.
“I’ve been able to pay for my nerve blocks with my GoFundMe – but I’m still raising money for some new camera equipment, and to be able to live independently.”
You can find Charlie’s GoFundMe via the link here.
If you’ve been affected by any of these issues and want to speak to someone in confidence, please don’t suffer alone. Call Samaritans for free on their anonymous 24-hour phone line on 116 123.
Featured Image Credit: (SWNS)

A doctor has issued critical advice on the key symptoms to look out for after a brand new variant of a ‘horrendous’ disease was confirmed to be present within the United Kingdom.
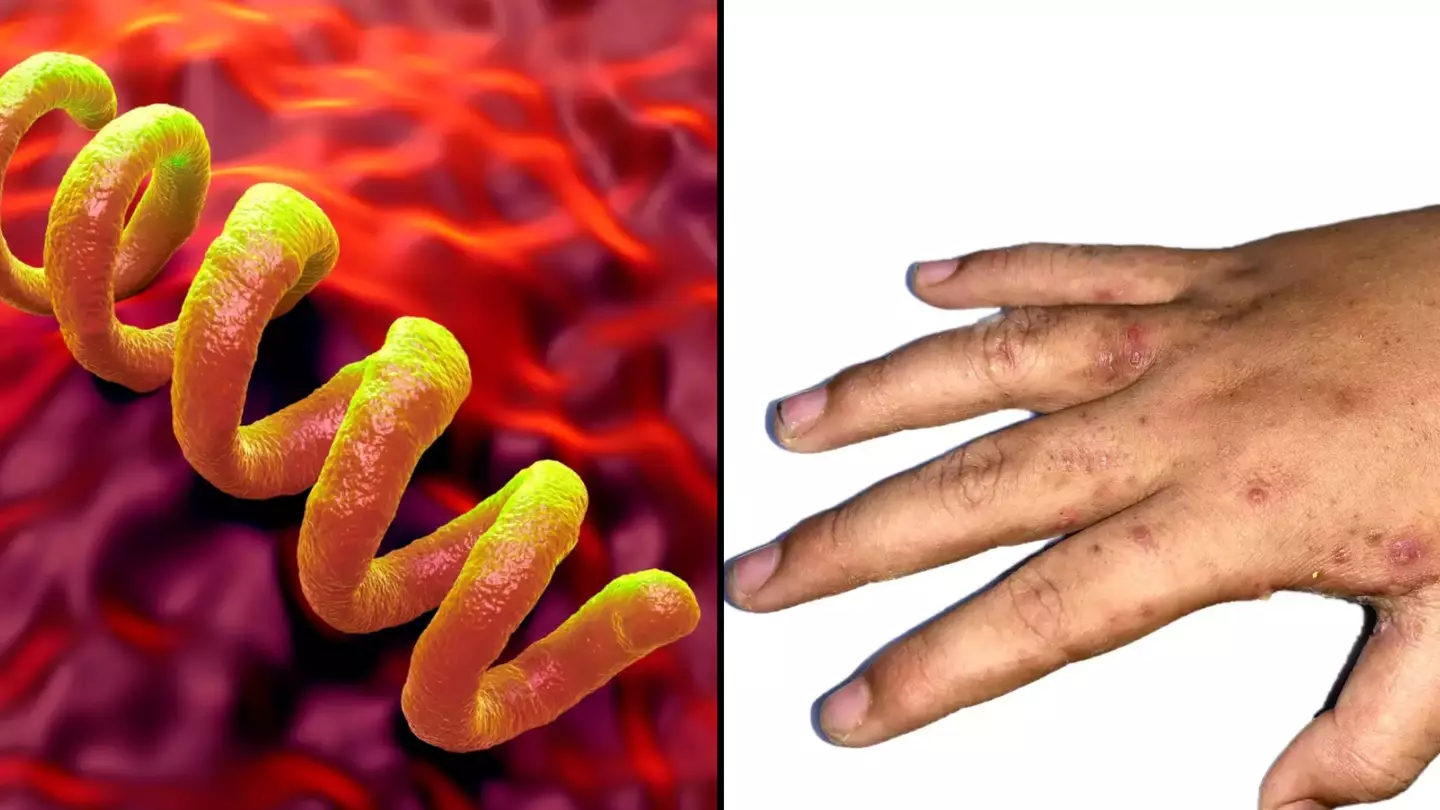
Mpox, which was known as monkeypox until 2022, has been confirmed in the UK, and there’s a brand-new variant of the potentially fatal disease now, which was found in one person in the country.
The variant, known as Clade 1b, was confirmed in the country by the UK Health Security Agency (UKHSA).
“This is the first detection of this Clade of mpox in the UK,” UKHSA says.
“It is different from mpox Clade II that has been circulating at low levels in the UK since 2022, primarily among gay, bisexual, and other men-who-have-sex-with-men (GBMSM).”

A rash is one of the early symptoms of mpox (Getty Stock Images)
Mpox global health emergency
It comes after the World Health Organisation (WHO) declared mpox a global health emergency in the summer of 2024.
The case of the mpox Clade 1b variant was confirmed in a UK patient who had recently returned from part of Africa, where the variant is currently spreading. He began feeling sick around a day after landing back in the country.
The case was detected in London, and the individual was transferred to the Royal Free Hospital High Consequence Infectious Diseases unit. No further details are being disclosed about the individual, UKSHA and the NHS says.
Professor Susan Hopkins, Chief Medical Adviser at UKHSA, said: “It is thanks to our surveillance that we have been able to detect this virus. This is the first time we have detected this Clade of mpox in the UK, though other cases have been confirmed abroad.
“The risk to the UK population remains low, and we are working rapidly to trace close contacts and reduce the risk of any potential spread. In accordance with established protocols, investigations are underway to learn how the individual acquired the infection and to assess whether there are any further associated cases.”

Blistering on the hands is a sign of mpox (Getty Stock Images)
Symptoms of mpox
Doctor John Burke, CMO of AXA Health, told LADbible about four main symptoms to look out for when it comes to mpox.
“Given there have been declared outbreaks of the virus in Africa, it’s understandable that the UK population may be worried about the virus spreading,” Dr Burke said.
“However, the risk to the UK population is currently low.”
The four common symptoms to keep an eye on are:
- The appearance of a rash that looks like blisters across the face and body
- High temperature and chills
- Headache, muscle aches, back pain, and a feeling of exhaustion
- Swollen lymph nodes
Dr Burke added: “These symptoms can be confused with other infectious illnesses, particularly chicken pox. At the current time in the UK, a history of travel to Africa or exposure to a known case are important features and advice from a health professional is needed if there are concerns.
“If you do contract the virus, it is usually mild and most people recover within a few weeks without any treatment, and there is an effective vaccine.”

Harun Tulunay in hospital with mpox (Harun Tulunay/WHO)
‘Horrendous high fever and pain, I couldn’t eat or move’
Harun Tulunay, from London, caught mpox in the summer of 2022 during the last major outbreak of the virus. Speaking about his experience to Sky News, Harun revealed that flu-like symptoms were the first to manifest.
Harun suffered from a high fever and muscle aches across his body.
After this, lesions and scars started to appear across his body.
He said: “After two weeks of horrendous high fever and pain, I wasn’t able to move or drink or eat anymore – at that point I was hospitalised.”
Harun received the mpox vaccination against future strains of the virus. Now, he wants it to be rolled out across the world, especially so in Africa, where infections are spreading worse than anywhere else.
Featured Image Credit: Getty Stock Images
Topics: Health, NHS, UK News, World News

Brits have been warned they may be mistaking an uncomfortable, Victorian-era skin disease with a more common condition.
As the colder days and longer nights draw in, you may begin to notice cuts and bumps on your ski,n and brush it off as a side effect of the chilly weather – but health experts are now warning to be mindful that your symptoms could point to something more sinister.
Enter scabies, a condition which was widespread during Victorian England.

According to health experts, these ‘Victorian’ conditions are on the rise (Getty Stock Images)
What is scabies?
According to guidance outlined by the NHS, scabies is a skin condition caused by mites burrowing into the skin, leading to an itchy rash in affected areas.
The main symptoms of scabies are intense itching – particularly at night – and a raised rash or spots, which will appear red on paler skin.
A scabies rash can spread across the whole body, but tends to impact skin around the fingers, wrists, underarms, and around the waist, groin, and bottom.
Scabies can infect anyone and is spread by close skin contact.
Nurseries, university halls, foe example, are places where you are at a higher risk of catching scabies.
If you catch scabies, it is important to wash all of your clothes and bedding at 60°C and keep your distance from other people to avoid spreading the condition.
What is the difference between scabies and eczema?
Due to its appearance and itchy sensation, Scabies can sometimes be mistaken for other skin conditions such as eczema, which is another inflammatory skin condition.
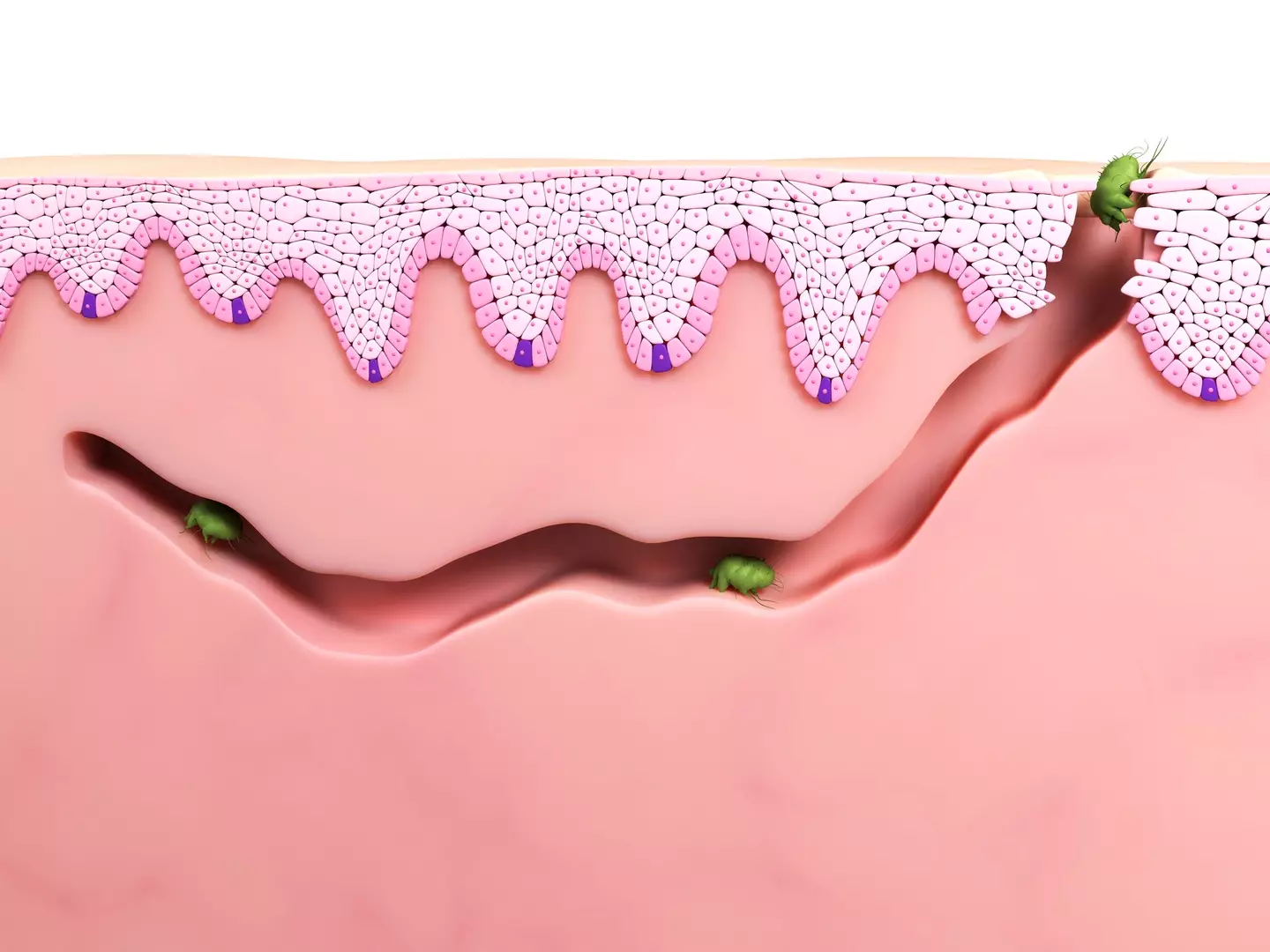
Scabies occurs when mites burrow under the skin (Getty Stock Images)
The key differences between the two conditions are:
- Scabies is infectious, whereas eczema is not
- Scabies is caused by mites, while eczema can develop due to various genetic and environmental factors
- Scabies and eczema have different treatment methods
- Eczema is typically found in the face, hands, feet, and elbows, whereas scabies can occur anywhere.
Having eczema cannot cause scabies, but having scabies can trigger an immune reaction which leads to you developing eczema.
It can also make existing eczema worse.
Why are ‘Victorian’ illnesses on the rise?
In recent weeks, GPs in the UK have warned Brits about a rise in transmission of ‘Victorian’ illnesses such as scabies, as well as scurvy and syphilis.
Dr Tess McPherson, of the British Association of Dermatologists, explained that a rise in scabies cases correlates with students returning to university, as well as people not isolating after developing symptoms (via The Times).

Conditions such as scabies, scurvy, and syphilis were common in the Victorian era (Getty Stock Images)
Meanwhile, chief medical officer Professor Sir Chris Whitty said a fall in public funding was responsible for making STI rates worse, adding that syphilis, another Victorian illness, has been on the rise, and is a ‘very dangerous disease with multiple complications’.
The report added that the third centuries-old condition to make a resurgence, scurvy, is likely being caused by people not getting enough fruit and vegetables, leading to vitamin C deficiency.
Featured Image Credit: (Getty Stock Images)
Topics: Health, UK News, World News
Around half a million Brits suffer from inflammatory bowel disease (IBD), an umbrella term from Crohn’s disease and ulcerative colitis.
Crohn’s disease can affect any part of the digestive tract, while ulcerative colitis causes inflammation of the large intestine.
The symptoms of IBD include stomach pain, diarrhoea, a sudden need for the toilet, blood in what comes out when you’re on the toilet, weight loss, fever and a lack of appetite.
Symptoms can also take a toll on your mental health, with anxiety and depression both being linked to inflammatory bowel disease as well.
In short, it’s an absolutely horrible thing to live with, and a woman who has IBD has explained what the absolutely worst thing about this smorgasbord of s**t is.

Researchers have found what could be a ‘holy grail’ breakthrough. (Getty Stock Photo)
Perhaps fortunately then, the cause of inflammatory bowel disease has been discovered by scientists in the UK in what could be a major breakthrough for a condition which affects around 500,000 Brits and a lot more people elsewhere in the world.
A study from Francis Crick Institute and University College London found that existing drugs seem to reverse IBD in cells and samples of patients.
Researchers are now working out how to make this medication specifically target the cells they’d need to tackle to deal with the likes of Crohn’s disease and ulcerative colitis.
27-year-old Lauren Golightly was diagnosed with Crohn’s in 2018 after developing stomach cramps and finding blood in her stool.
As you might imagine, she’s a big fan of this news.

A woman diagnosed with Crohn’s disease in 2018 said the research was ‘exciting and encouraging’. (Francis Crick Institute)
“Crohn’s has had a huge impact on my life. I’ve had a rocky road since diagnosis, with many hospital admissions, several different medications and even surgery to have a temporary stoma bag,” she said, before moving on to discuss the worst thing about it.
“One of the hardest things about having inflammatory bowel disease is the uncertainty around it.
“I still experience flare-ups and can still spend quite a bit of time in hospital. Learning about this research is so exciting and encouraging.
“I am hopeful this could potentially make a difference for myself and so many other hundreds of thousands of people living with IBD.”
This latest development has been dubbed a ‘holy grail’ discovery and it’s hoped that clinical trials on humans could begin at some point in the next five years.

Around half a million Brits suffer from inflammatory bowel disease. (Getty Stock Image)
Some work is still to be done on the existing drugs we have, but it’s a big step in the right direction.
James Lee, group leader of the Genetic Mechanisms of Disease Laboratory at the Crick, and consultant gastroenterologist at the Royal Free Hospital and UCL, who led the research, said: “IBD usually develops in young people and can cause severe symptoms that disrupt education, relationships, family life and employment. Better treatments are urgently needed.
“Using genetics as a starting point, we’ve uncovered a pathway that appears to play a major role in IBD and other inflammatory diseases.
“Excitingly, we’ve shown that this can be targeted therapeutically, and we’re now working on how to ensure this approach is safe and effective for treating people in the future.”
Featured Image Credit: Francis Crick Institute/Getty Stock Images
The best ways to avoid and control the spread of a Victorian disease sweeping the UK at the moment have been revealed.
As Britain gets darker and colder in the lead-up to Christmas, people may notice cuts and bumps on their skin all of a sudden.
While some might think it’s due to the drop in temperature, it could be down to scabies, a condition which was once widespread throughout Victorian England.

GPs are ‘seeing a spike in cases’ in the UK (Getty Stock Image)
Professor Kamila Hawthorne, chair of the Royal College of GPs, told the BBC that the number of GP diagnoses was ‘above the five-year average and rising, with the north of England seeing a spike in cases’.
Notably, scabies is not the same thing as eczema, but it can make it worse.
The key difference is that scabies is infectious, whereas eczema is not.
What is scabies?
Scabies is an itchy rash caused by mites and is mainly spread through close skin contact.
The NHS recommends that scabies ‘should be treated quickly to stop it spreading’, even though it ‘is not usually a serious condition’.
“While not a serious condition, scabies can be very itchy and irritating,” Professor Hawthorne added.
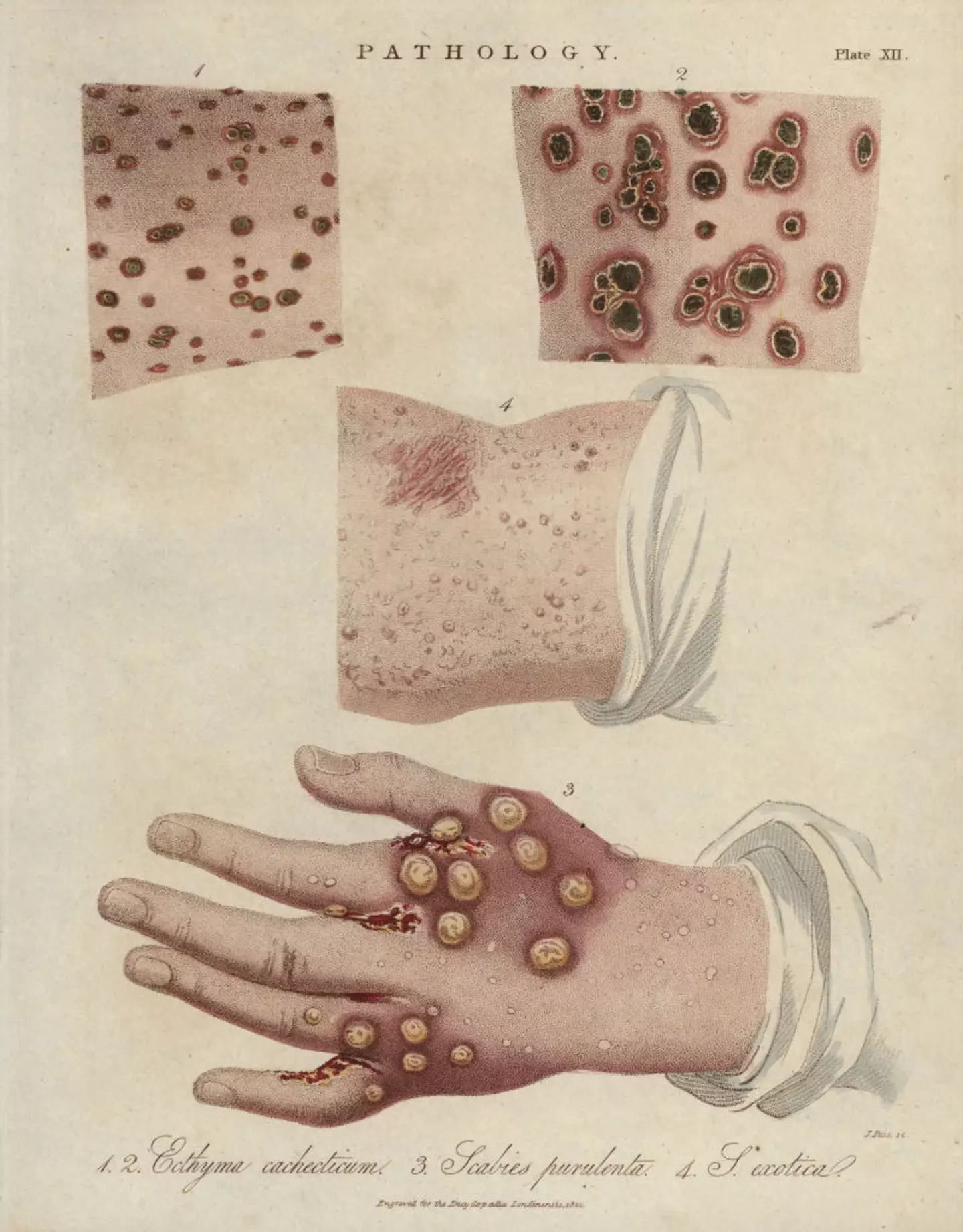
Scabies is a condition which was widespread during Victorian England (Florilegius/Universal Images Group via Getty Images)
“If not properly treated, it can spread and increase a patient’s risk of complications, such as secondary skin infections or make existing skin conditions worse.
“We recognise that patients may be apprehensive to seek treatment given the social stigma that surrounds the condition, but it is important that they don’t ignore their symptoms as this could lead to them getting worse and risks transmitting the condition to other people.”
Dr Ross Perry, GP and medical director at Cosmedics Skin Clinics, describes scabies as ‘an incredibly uncomfortable itchy and bumpy rash’ and that the symptoms are caused by ‘the saliva, eggs and faeces of the parasite mite sarcoptes’.
“Scabies rash can actually take up to eight weeks to appear on the body, during which time it can be spreading at an alarming rate, particularly on bedding, towels and clothes,” he said.

Scabies can spread to any part of the body (Getty Stock Image)
Best way to avoid the spread of scabies
According to America’s science-based health help service CDC, there are a number of things you need to do to control the spread of scabies:
- Be sure to treat all household members who are infected with the disease at the same time to avoid it spreading.
- Wash all clothing and bedding used during the three days before treatment started. Clothing should be machine-washed using hot water, dried on the hot cycle, or dry-cleaned.
- Temperatures in excess of 50°C for 10 minutes will kill mites and eggs.
- If you can’t wash or dry clean an item, store it in a closed plastic bag for several days to a week to disinfect it.
Featured Image Credit: Getty Stock Images
